Huddled, crying on the bathroom floor, laying in bed for days or smiling on until the bullet hits, depression lives in the minds of millions. The disorder holds the potential to completely debilitate people. Mental illnesses and disorders such as anxiety, post-traumatic stress disorder(PTSD), schizophrenia, obsessive-compulsive disorder (OCD) and depression affect 1 in 5 American adults. These disorders influence people to seek medical care, which in severe cases includes hospitalization.
Americans consider plummeting mental health as a crisis in this country that deeply affects minorities and those living in poverty. After 2020, upticks in depression, anxiety and suicide, notably in young people, led to this increase in concern. These upticks likely arose from the pandemic’s effects on job loss and isolation. Unfortunately, history shows that although help remains prevalent and effective, in certain cases, the structure of mental rehabilitation can not consistently provide what the system promises.
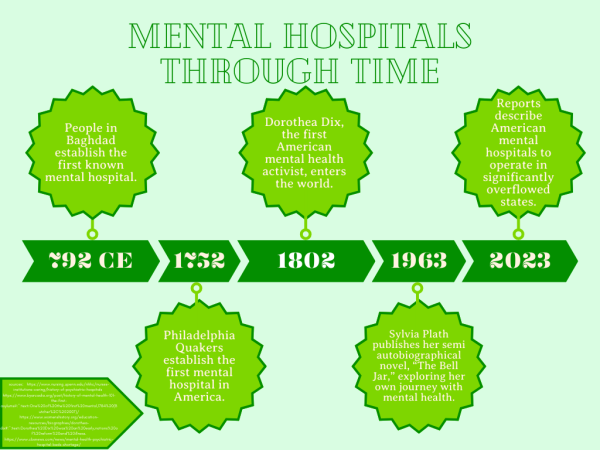
Historically, psychiatric hospitals or asylums have operated with good intentions, yet imperfectly. Mental hospitals in the 18th century used isolation and the unexpected dunking of patients in ice-cold water to treat disorders such as mania and melancholia when families and communities no longer could support their loved ones who lived with mental illness. The Quakers in Philadelphia established the first American institution in 1752—the building included a dimly lit basement, decked out with clinking shackles on the walls. Demand for the hospital’s treatments stood so high that shortly after its inception, it expanded. Following the Quaker’s hospital, several other wards sprung up across America in the 18th and 19th centuries. A portion of these new institutions utilized “moral treatment”— a European technique much less severe than former methods of treating people with mental illness. Unfortunately, due to the overpopulation of the hospitals, the hospitals could no longer assist the patients effectively. By the end of the 19th century, insane asylums transformed into beaches for women to wash up, should they dare think independently.
Even moving into the 20th century, people living with mental illness struggled to locate a decent hospital, as inferior treatment practices ran rampant throughout the institutions. The 1950s became rather infamous for this tendency due to a common perpetuation of out-of-date tactics. These tactics notably included lobotomies and long-term stays in mental hospitals. Poet and author Sylvia Plath immortalized this reputation in her semi-autobiographical novel “The Bell Jar”. Through her character Esther, she explores her struggles with depression in the 1950s and her own experience with poorly administered electric shock therapy—a treatment that she portrayed as both traumatic and ineffective. She also describes her time in two highly differing mental hospitals: one, a public hospital which she found incredibly distressing; and two, the private, more helpful, McLean Hospital.
Modern mental hospitals aim to quickly help people living with mental illness take on a path to recovery. Although long-term care exists, the majority of inpatient mental health care typically lasts a week or two. Hospitals made this switch to quicker treatment after deinstitutionalization in the mid-20th century. Although the deinstitutionalization movement was originally meant to move mental health patients from hospital to familial and community care, the short length of stays in mental hospitals transitioned its main effect today. Despite the brief time expected of hospital stays, the need for hospitalization only applies to those in a crisis, essentially meaning those who may pose a risk to themselves or others. The facility helps to quickly and efficiently provide therapeutic and medicinal help until a patient’s symptoms stabilize. Mental hospitals provide a safe haven for people to recover from a crisis so they can move to long-term treatments for their symptoms, such as therapy. These outpatient treatments do not disrupt a patient’s life as much as a long-term inpatient stay in a mental hospital would. The difference in day-to-day life disruption rests chiefly in the flexibility offered by outpatient care, such as therapy, rather than overnight, day or week-long time commitments inherent in inpatient facilities.
“Mental health hospitals allow the individual in distress to be removed from their current environment to one of healing and support. That support comes in the ways of mental health associates, nurses, doctors, recreation therapists, nurse practitioners, and mental health counselors. While in the healing environment, the individual receives medication management, and individual, group and family therapy. Social workers assist the individual in setting up services in the community to continue the healing journey,” Laurel Heights Hospital Director of Clinical Services Bekah Fisher said.
People become patients in a mental hospital for reasons such as suicidal thoughts or attempts, severe depression, mania, paranoia, self-harm and urges to harm others. While in the hospital, treatments attempt to balance the patient’s chiefly pressing issues through medication, therapy and various activities. Although patients’ experiences reflect unique situations and individual hospitals, according to a study conducted by the United States National Mental Health Services Survey (N-MHSS), approximately 26.5% of patients gave American mental hospitals a five-star review, reaffirming that their stay proved helpful and necessary for their recovery. In cases in which mental illness poses a risk to the individual or public, such as severe depression that can lead to suicidal thoughts or schizophrenia which can contribute to violent behavior, the programs offered by a mental hospital permit doctors to assess the need for treatment such as medication and types of therapy that could lead to the patient’s recovery.
“I would only recommend in-patient treatment to a patient that I was concerned we could not maintain their physical safety in a nonclinical setting or if the patient is detoxing from a substance that needs to be medically monitored. In most cases with my patients, I have found that supporting the patient and their natural supports (immediate family/spouse) during a crisis helps the patient feel empowered… whereas sometimes hospitalization can create an unhealthy coping pattern that patients might turn to over and over again when they experience similar triggers leading them to feel like they are not safe and able to safely exist outside of hospitalization,” Licensed Professional Counselor at Harvest Counseling Katie Toso said.
Following the 2020 pandemic, mental health quality significantly decreased in teens and adults alike. According to the CDC, the number of people who received mental health treatment increased from 19.2% in 2019 to 21.6% in 2021. Due to this emotional strain, mental hospitals struggled to accommodate the increase in patients. A hospital bed shortage crisis ensues; in situations where room remains, the lack of sufficient mental health professionals frequently prevents the entry of people seeking help, or results in inferior care. This obstruction to entry can cause a magnification of patients’ symptoms.
As hospitals stretch beyond their capacity, mental hospitals struggle to maintain enough staff to properly care for their patients. As of February 2023, American hospitals reported using 144% of inpatient beds for psychiatric treatment. The struggle to acquire enough beds to meet the demand for psychiatric inpatient care leads to the need for patients to travel in search of care or to settle for lower-quality places. Unfortunately, even with an increase in physical beds, the struggle to staff psychiatric hospitals continues.
“There have been a number of hospital systems that have created more beds for mental health, my own included. The difficulty is staffing. It’s very difficult. There’s just a terrible shortage of people qualified to do this work who are willing to do it,” Sandra M. DeJong MD, a pediatric psychiatrist at Cambridge Health Alliance in Harvard Medical School, said.

With patients rarely staying more than a week or two in a mental hospital, today’s facilities prioritize a quick process. Days consist of group therapy, individual therapy, art, the administration of medicine and time for patients to spend freely within the constraints of the hospital. While the shorter periods and highly regulated activities keep patients safe short-term, the briefness can limit individualized treatments and make patients feel not properly cared for. Hospitals prioritize ensuring that treatments specifically cater to the patient’s needs because people who live with mental illness each live a unique story, and the illness manifests vastly differently as a result. Truly, professionals struggle to successfully assist someone struggling with mental health in a week or less when the hospital does not employ a full staff or the number of patients overwhelms it.
“Many of my friends have gone to a mental hospital. I can’t personally speak on whether their mental health has improved, but most of them have said that it didn’t improve their mental health instead just taught them to hide it more. I do not think that a mental hospital would help me. Mental hospitals make patients feel ashamed for their mental issues instead of supporting and helping them,” sophomore Margaret Hollister said.
Additionally, psychiatric hospitals enforce a myriad of rules regarding patient clothing such as regulating hoodie strings, jewelry and shoelaces to avoid patients attempting self-harm or suicide. Nonetheless, the taking of one’s clothes or checking for smuggled items may result in the removal of a patient’s dignity, particularly when facilities issue patients hospital gowns because dignity depends so greatly upon freedom of choice, embodied by what one chooses to wear. Experts even argue that—in certain situations— hospitals should prioritize dignity over the protection of health. Contributions to feelings of dehumanization do not stem exclusively from rules, but also the staff’s patient treatment. Although each person who works at a mental hospital behaves uniquely, in an anonymous survey conducted by The Chant, 100% of NC students who have visited or know someone who has visited a mental hospital described their stays as neutral to awful due to the staff shortage and the actions of the overstretched staff.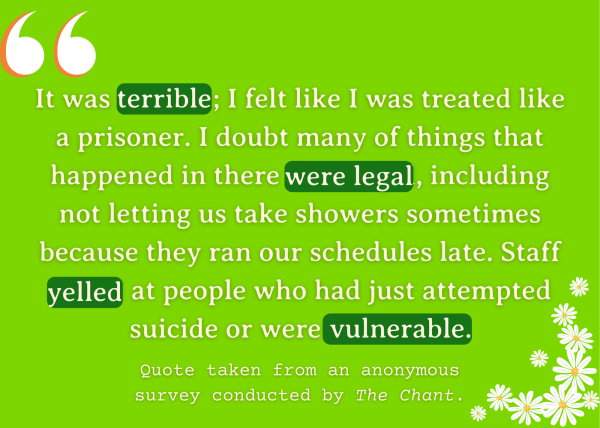
When people need treatment for mental disorders, roadblocks beyond issues within individual facilities may prevent them. The system for financing patients’ stays in American hospitals poses a problem people with mental illness face when seeking treatment. The price of a stay in a mental hospital can vary widely depending on the types of treatment, length of stay and location; uninsured patients may need to pay above 1000 dollars for each night. The majority of private mental hospitals do not accept insurance and can cost upwards of $30,000 each month. Although, legally, hospitals may not refuse care to patients who meet inpatient treatment requirements, the financial burden can still significantly deter or financially burden those who cannot comfortably afford care. Furthermore, people who experience mental illness will not likely seek it out if it will cause a financial burden.
“Long ago, mental health hospitals had more time to work with individuals and their families (if applicable). Now, mental health workers fight with insurance companies to have more time to treat their patients. The idea of “long-term treatment” and “padded rooms” are outdated. We live in a world of managed care and it’s our responsibility to provide the highest quality of care even in working within a short time frame,” Laurel Heights Hospital Director of Clinical Services Bekah Fisher said.
To combat the problems that occur within psychiatric hospitals, the US government can take action to ensure people’s rights to life and happiness. The government can accomplish this reform in two ways. Congress can allot money to a Medicaid-adjacent program aimed at helping unemployed and poor people receive medication, therapy, inpatient care and other forms of care, and they could provide benefits to people working in the field or receiving the necessary education to work in it. Ensuring the quality and accessibility to mental health care, particularly mental hospitals, does not come with ease, but the necessity to keep people safe outweighs the difficulties.
The importance of mental health care does not lose its legitimacy purely because of problems within the system. If anyone struggles with mental health, they can receive the necessary help. No two locations or services treat patients the same, so people living with mental illnesses absolutely can and should find the right fit.












Amy Winehouse • Jan 5, 2024 at 1:27 PM
Lovely! I could feel your passion for writing though the power of your words. This is so amazing. I wish I could give you more than five stars. Keep up the great work young lady! I am so proud of you.