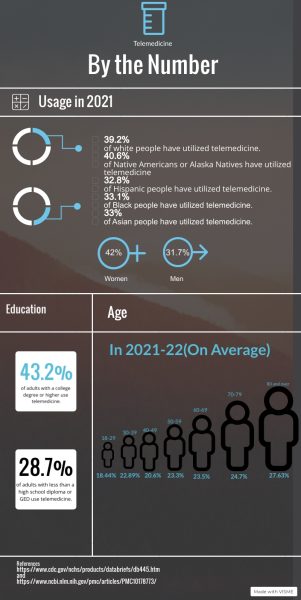
After the COVID-19 pandemic hit nations worldwide, people held one wish and one wish only: to stay as far away as possible from other people. This desire led to a change in people’s everyday activities, especially after the government implemented social distancing. Even with a nationwide lockdown issued by former president Donald Trump, between 80, 000 and 180,000 American nurses and doctors died from the virus. To keep healthcare providers safe, telemedicine—healthcare services delivered electronically— became highly prevalent to assist people with less serious health matters that did not require in-person attention. Doctors and nurses have worked with patients who may live hours away, who do not feel comfortable sitting near other sick patients or who find themselves too busy to take a trip to a medical office. Despite its positive intentions, sufficient controversy has emerged over the risks and benefits of telemedicine.
The Greek and Latin term telemedicine translates to “healing at a distance.” Thomas Bird, who referred to telemedicine as the delivery of medical assistance via telecommunication devices, coined this term in the 1970s. The first recorded use of telecommunications to report health-related concerns appeared during the Civil War. The telegraph allowed the Union Army to order medical supplies, to report injuries on the battlefield and to record casualties. In 1959, clinicians at the University of Nebraska utilized video communication to transmit neurological examinations across campus to medical students. As a result, universities across the nation utilized telemedicine, mainly focusing on transmitting medical data such as X-rays, electrocardiograms(ECG) and stethoscope sounds.
When discussing virtual healthcare, people may confuse telemedicine and telehealth. Telemedicine refers to remote clinical services such as a doctor’s appointment occurring online; telehealth refers to remote non-clinical services, such as providing training, continuing medical or public health education and electronic information sharing to facilitate and support assessments. Patients will likely resort to telemedicine rather than telehealth. For example, telemedicine would work best for a patient seeking medical attention for a condition such as a yeast infection. Although two different meanings, telemedicine and telehealth professionals can collaborate to provide patients with comfortable and speedy healthcare.
Private insurance plans can cover the cost of telemedicine services, but the amount of coverage depends on one’s plan. Similar to an in-person visit, one may also engage in a copay for a virtual appointment. If insured by Medicare, one must meet certain requirements to receive coverage for telehealth and telemedicine services. Medicare, however, has expanded telemedicine coverage due to COVID-19. Certain Medicare Advantage plans may provide greater telemedicine benefits than original Medicare.
Telemedicine can consist of holding doctor office appointments via Zoom calls, consultations via telephone and advanced procedures such as telesurgery where surgeons receive visual information so robots can perform surgical procedures. Other main types of telemedicine include store-and-forward telemedicine and remote patient monitoring. Store-and-forward telemedicine transfers data through laboratory reports, images and sounds among patients and doctors. This type of telemedicine increases efficiency and enlists expedited patient outcomes, which leads to swifter and improved patient results. Remote patient monitoring involves patients wearing heart monitors, skin patches, smart shoes or smartwatches to gather significant health data. These devices have led healthcare practitioners to make well-informed and accurate decisions; they also yielded an increase in recovery rates.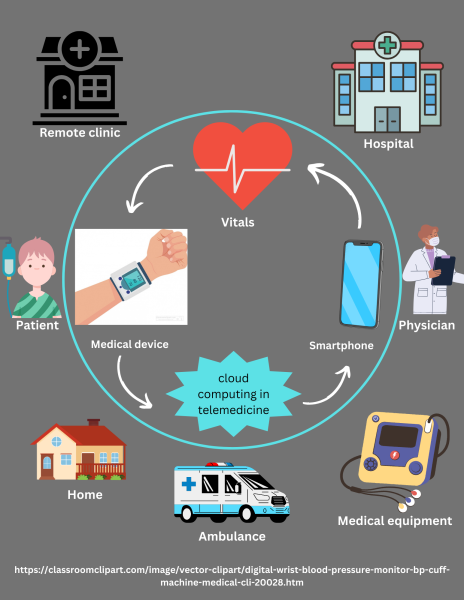
“Online healthcare will provide us immediate assistance and provide us with our needs at the touch of a screen instead of in-person which causes clutter in a medical space and infects others. As of now, doctors are already doing online appointments like Zoom calls to check up on their patients. I feel like online healthcare is beneficial because it will make me feel more comfortable. After all, I can deal with a minor issue at home and won’t have to worry about getting sick by others,” certified nurse assistant in training at Kennesaw State University NC senior Christine Olivera said.
Since the late 1900s, Americans from urban and rural areas have used technology to connect with others; this number has increased by 26.6% from 2020 to 2021. From Zoom calls for work, connecting with a long-distance loved one and even yoga classes, the video conferencing platform exceeded $100 billion during the pandemic, a 383% increase on its value in January 2020. Zoom works with Electronic Health Record (EHR) programs, such as Epic and Cerner to allow providers to schedule and join virtual appointments. Patients can use medical devices that work with Zoom to send real-time examination data such as heart rate, body temperature and videos of different body parts to their provider. Moreover, Zoom promotes better health outcomes and increased healthcare.
“Telemedicine is very convenient, it saves time, and it is more cost-effective than seeing patients in person. It allows for better patient follow-up and allows providers to reach more patients. Telemedicine has impacted the public health community by increasing access to healthcare for patients who are unable to be present in person because of distance or transportation issues. Telemedicine allows healthcare providers to reach more people, can reduce time in making an in-person diagnosis, and overall allows for better healthcare choices,” staff director at the Food and Drug Administration(FDA) and commander of the United States Public Health Service Nicole Bell said.
Correctional facilities also utilize telemedicine to ensure the safety of those incarcerated. Despite the prevalence of telemedicine within the last three years, it has existed in correctional facilities as early as 2013. Jails and prisons use telemedicine to help people with mental illnesses and substance use disorders. Prisoners who wish to seek the reentry process hold virtual appointments with counselors who prepare prisoners to continue their growth outside of the correctional facility. Telemedicine also helps veterans who do not hold access to proper healthcare due to geographical and economic disadvantages. Within the military, doctors utilize telemedicine to aid the wounded and guide veterans through physical and mental rehabilitation.
Opponents of telemedicine believe a virtual appointment excludes the intimacy and security they would receive in an in-person appointment. For personal appointments, such as visiting an obstetrician-gynecologist(OBGYN), one might feel more at ease if this appointment occurred in person rather than virtually. When testing out a new doctor, people may feel more comfortable if they meet with a doctor in person, so they can observe their environment and build trust. Ultimately, telemedicine has come a long way since the 20th century and has also yielded favorable results. As the world begins to technologize, telemedicine will likely become increasingly prevalent in everyday lives.
While telemedicine has opened doors for those who reside in rural communities and people who experience anxiety while at the doctor’s office, it also comes with drawbacks. Telemedicine’s qualities can achieve various healthcare goals, but in certain cases, it cannot fully assist patients. The practice includes limitations on performing physical examinations, security breaches and regulatory barriers. Medical professionals cannot examine a patient physically, thus leading to inaccurate diagnosis and jeopardizing a patient’s health.